Improving Bispecific Antibodies for Efficacy and Safety in Multiple Myeloma
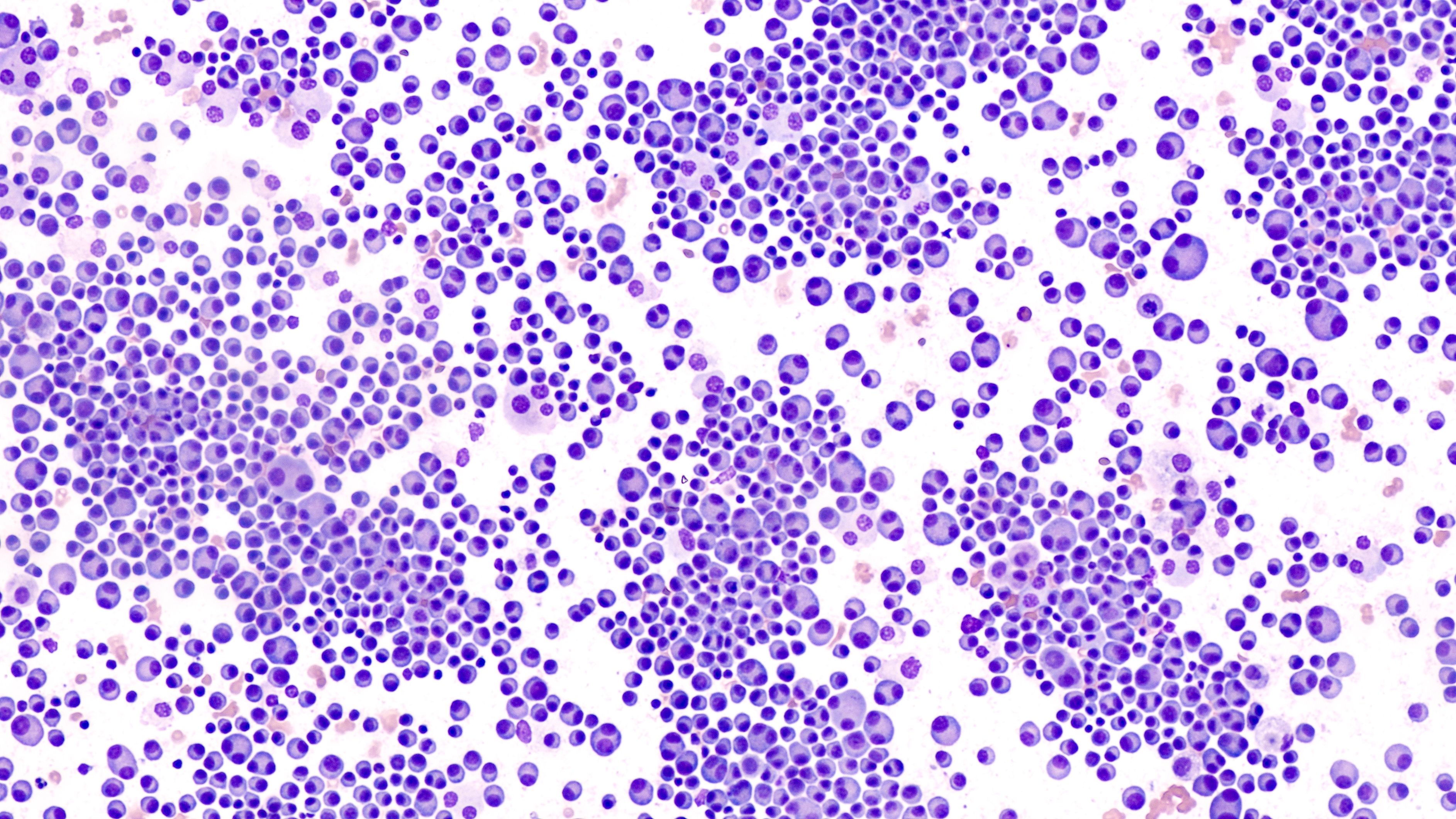
Bispecific antibodies are transforming the management of relapsed or refractory multiple myeloma, offering hope for improved outcomes and innovative treatment strategies. Ongoing research is focused on enhancing the use of these antibodies in earlier stages of treatment and addressing potential side effects. To successfully integrate bispecific antibodies into oncology care, considerations for facility readiness and patient selection are crucial.
During the Hematology/Oncology Pharmacy Association Annual Conference 2024 in Tampa, Florida, Kirollos Hanna, PharmD, discussed key considerations for operationalizing bispecific antibodies in the treatment of relapsed or refractory multiple myeloma. Hanna highlighted the success of teclistamab-cqyv and its impact on patient response rates compared to previous treatment options. The promising efficacy profiles of bispecific antibodies like teclistamab-cqyv, talquetamab, and elranatamab suggest a positive trend in improving outcomes for multiple myeloma patients.
Clinical trials are exploring innovative strategies to combine different mechanisms targeting B-cell maturation antigen (BCMA) and G protein-coupled receptor, class C, group 5, member D (GPRC5D) to enhance treatment responses. These trials are also evaluating dose modification strategies and investigating additional targets within multiple myeloma and other hematologic cancers. The potential for bispecific antibodies to be used in earlier lines of therapy indicates a shift towards proactive treatment approaches to benefit patients with multiple myeloma.
In terms of safety profiles, bispecific antibodies such as teclistamab-cqyv, blinatumomab, and tebentafusp share common side effects like cytokine release syndrome (CRS), immune effector cell-associated neurotoxicity syndrome (ICANS), neurotoxicities, and infections. However, variations in the severity and incidence of adverse events exist among these therapies. Considerations for logistics, staff training, and facility readiness are essential when incorporating these therapies into patient care.
Each bispecific antibody may present unique challenges operationally. For instance, blinatumomab requires a continuous infusion method, while teclistamab-cqyv involves subcutaneous injections. These differences in administration may impact logistical considerations for healthcare systems. Understanding the nuanced adverse events associated with each therapy, such as taste changes and weight loss with talquetamab, is vital for effectively managing patient care.
Overall, the evolution of bispecific antibodies in the treatment of multiple myeloma offers hope for improved patient outcomes and enhanced treatment strategies. By addressing facility readiness, patient selection, and potential side effects, healthcare providers can optimize the use of bispecific antibodies in oncology care to provide better outcomes for patients with relapsed or refractory multiple myeloma.